Sleep apnea is a serious sleep disorder that can have significant impacts on your health and quality of life. If you suspect you might have this condition, seeking a thorough evaluation is essential. In Melbourne, numerous sleep clinics offer testing and treatment options, but choosing the right one can be challenging. This article will guide you through understanding sleep apnea, the importance of testing, how to choose a sleep clinic, preparation for testing, and interpreting your results.
Understanding Sleep Apnea
What is Sleep Apnea?
Sleep apnea is a sleep disorder characterized by repeated interruptions in breathing during sleep. These interruptions can last from a few seconds to minutes and may occur dozens or even hundreds of times a night. The most common form is obstructive sleep apnea (OSA), which occurs when the muscles at the back of your throat fail to keep the airway open.
Getting tested for sleep apnea test Melbourne is vital for various reasons. Firstly, it can confirm whether you have the disorder and identify its severity. Testing is also essential to rule out other potential sleep disorders that may present similar symptoms.
Another form is central sleep apnea, which is less common and involves a failure of the brain to send proper signals to the muscles that control breathing. Complex sleep apnea syndrome, a combination of both obstructive and central sleep apnea, is also possible. Understanding these distinctions is vital for effective diagnosis and treatment, as the management strategies can differ significantly based on the type of sleep apnea a patient is experiencing.
Symptoms and Risks of Sleep Apnea
Common symptoms of sleep apnea include loud snoring, gasping or choking during sleep, excessive daytime sleepiness, difficulty focusing, and mood changes. These symptoms can significantly interfere with your daily life and overall health. Additionally, many individuals with sleep apnea may not even be aware of their condition, as they often do not remember waking up during the night. This lack of awareness can lead to a prolonged delay in seeking treatment, exacerbating the associated health risks.
The risks associated with untreated sleep apnea are severe. They can lead to cardiovascular problems, high blood pressure, diabetes, and even increased likelihood of accidents due to daytime drowsiness. Furthermore, sleep apnea has been linked to complications such as stroke and heart failure, making it essential to address the disorder promptly. The impact of sleep apnea extends beyond physical health; it can also affect mental well-being, contributing to anxiety and depression. Recognizing symptoms and seeking help is crucial to mitigate these health risks, and early intervention can lead to improved quality of life and overall health outcomes.

The Importance of Sleep Apnea Testing
Why Get Tested for Sleep Apnea?
Proper diagnosis allows for a targeted treatment approach. Instead of self-diagnosing or relying on anecdotal evidence, testing provides a scientific basis for understanding your sleep health. Effective treatments can improve your quality of life significantly, making testing an indispensable step. Moreover, untreated sleep apnea can lead to serious health complications, including cardiovascular issues, diabetes, and even cognitive decline. By addressing the disorder early through testing, you can mitigate these risks and enhance your overall well-being. Find more about cognitive on https://www.cognitioneducation.com/
The Role of Sleep Clinics in Diagnosis
Sleep clinics are specialized facilities equipped to conduct comprehensive assessments of sleep disorders. They employ a team of professionals, including sleep specialists, respiratory therapists, and polysomnographic technologists, to oversee your sleep study.
At a sleep clinic, various diagnostic tools are used to monitor your sleep patterns, oxygen levels, and overall sleep quality. These clinics provide a supportive environment where you can discuss your concerns openly with experts who understand the complexities of sleep apnea. In addition to traditional overnight sleep studies, many clinics now offer home sleep apnea testing options, making it more convenient for patients to receive the necessary evaluations. This flexibility ensures that more individuals can access the care they need, regardless of their circumstances. Furthermore, the data collected during these assessments can lead to personalized treatment plans that cater specifically to your unique sleep patterns and health needs, ultimately fostering a more effective path to recovery and restful nights.
Learn about sleep apnea test with medicare on: Sleep Apnea Test with Medicare
Choosing the Right Sleep Clinic in Melbourne
Factors to Consider When Choosing a Sleep Clinic
When searching for the right sleep clinic in Melbourne, there are several factors you should consider:
- Accreditation: Ensure the clinic is accredited by relevant health organizations, confirming it meets specific standards of care.
- Specialization: Look for clinics that specialize specifically in sleep disorders rather than general health facilities.
- Reputation: Research online reviews and testimonials to gauge patient satisfaction and the clinic’s overall reputation.
- Technology: Inquire about the technology and equipment used during testing, as newer and more advanced tools often lead to more accurate diagnoses.
- Follow-up Care: Check if the clinic offers follow-up consultations to help manage your treatment after diagnosis.
What to Expect from a Reputable Sleep Clinic
Upon choosing a reputable sleep clinic, you can expect a comprehensive evaluation process. Initially, you will likely undergo a consultation to discuss your symptoms and medical history. This step is crucial in tailoring the testing to your needs.
During your sleep study, you should feel comfortable and monitored. The environment should be conducive to sleep, allowing for an accurate representation of your typical sleeping patterns. Staff will be available to answer your questions, and you should receive regular updates on results and next steps following your test.
In addition to the initial consultation and sleep study, many clinics offer educational resources to help you understand your condition better. This could include workshops or informational sessions that cover various sleep disorders, treatment options, and lifestyle changes that can improve sleep quality. Having access to these resources can empower you to take an active role in your treatment journey, making it easier to implement recommendations from your healthcare provider.
Furthermore, the clinic’s approach to treatment can vary significantly. Some clinics may focus on cognitive behavioral therapy for insomnia (CBT-I), which has been shown to be effective for many patients. Others may emphasize the importance of sleep hygiene practices, such as maintaining a consistent sleep schedule and creating a restful sleeping environment. Understanding the clinic’s philosophy on treatment can help you align your expectations and ensure that you receive care that resonates with your personal health goals. To read more about therapy click here.
Preparing for Your Sleep Apnea Test
How to Prepare for a Sleep Study
Preparation for a sleep study is relatively straightforward but requires attention to detail. Here are some steps to follow:
- Avoid Stimulants: Refrain from caffeine and nicotine at least 12 hours before your study, as these can affect your ability to fall asleep.
- Maintain Your Routine: Try to stick to your regular sleep schedule as much as possible in the nights leading up to the test.
- Discuss Medications: Inform your doctor about any medications you are taking, as some may need to be adjusted before the study.
- Wear Comfortable Clothing: Choose loose-fitting clothing to ensure comfort during the night.
Understanding the Sleep Apnea Testing Process
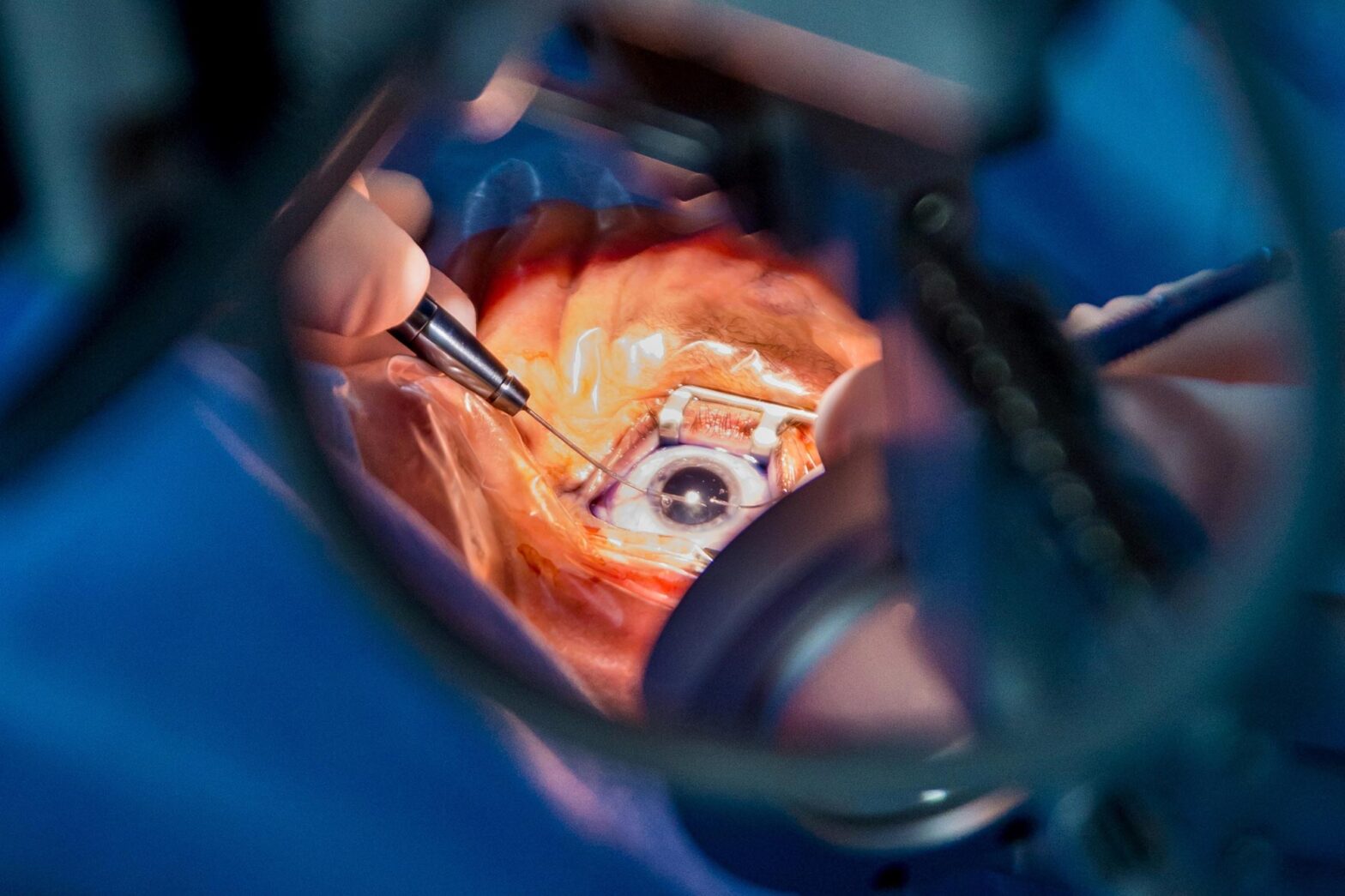
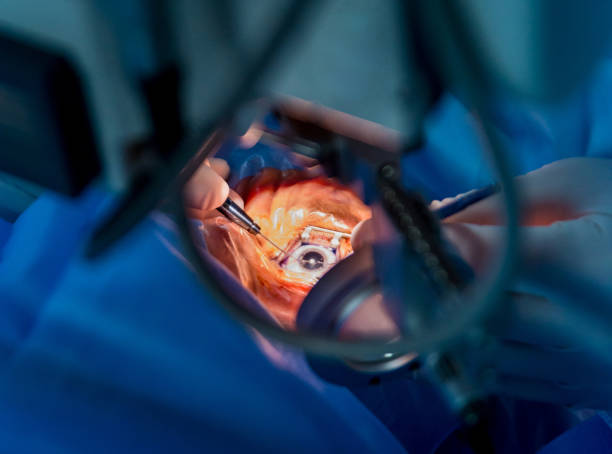
The sleep apnea testing process, often referred to as a polysomnography, involves monitoring various physiological functions while you sleep. This includes brain activity, eye movements, heart rate, respiratory effort, and blood oxygen levels.
During the test, sensors will be attached to your body, which may feel unusual, but they are painless. The data collected overnight is analyzed by sleep specialists to identify any apneas or hypopneas (shallow breathing patterns) and to understand your overall sleep architecture.
It’s important to note that the environment in which the sleep study takes place is designed to be as comfortable as possible. Many facilities offer private rooms with adjustable lighting and temperature controls, allowing you to create a sleep-friendly atmosphere. You may also be encouraged to bring personal items such as a favorite pillow or blanket to help you feel more at ease. This familiarity can significantly impact your ability to relax and fall asleep during the test, leading to more accurate results.
Additionally, the duration of the sleep study can vary. While many tests are conducted overnight, some may require extended monitoring, especially if you have complex sleep issues. In such cases, the staff will explain the process in detail, ensuring you understand what to expect. This transparency helps alleviate any anxiety you may have about the procedure and reinforces the importance of the data collected in diagnosing and managing your sleep apnea effectively.

Interpreting Your Sleep Apnea Test Results
What Do Your Test Results Mean?
Test results provide valuable insights into whether you have sleep apnea and, if so, its severity. Results are usually reported in terms of the Apnea-Hypopnea Index (AHI), which counts the number of events per hour of sleep.
An AHI score of fewer than five is considered normal, while mild sleep apnea ranges from five to fifteen, moderate from fifteen to thirty, and severe cases involve thirty or more events. Understanding these results is crucial for determining the appropriate treatment options. Additionally, your test may also reveal other important metrics, such as oxygen saturation levels and the duration of apneas, which can further inform your healthcare provider about the impact of sleep apnea on your overall health.
For instance, a significant drop in oxygen saturation during sleep can indicate that your body is struggling to get enough oxygen, which can lead to various health complications over time, including cardiovascular issues. Therefore, it’s essential to not only focus on the AHI score but also to consider these other factors when interpreting your results.
Next Steps After Receiving Your Test Results
After receiving your test results, you will typically have a follow-up appointment with your sleep specialist to discuss the findings. Together, you will explore treatment options, which may include lifestyle changes, CPAP therapy, oral appliances, or even surgical interventions in more severe cases.
It is essential to be proactive in discussing any concerns and following the treatment plan prescribed. Regular follow-ups may be necessary to monitor your progress and adjust the treatment as needed. Your doctor may also recommend additional tests or evaluations, such as a sleep study in a different setting or a home sleep apnea test, to further assess your condition and ensure that the chosen treatment is effective.
Moreover, it’s important to consider the psychological and emotional aspects of living with sleep apnea. Many individuals experience anxiety or depression related to their condition, which can affect their overall well-being and adherence to treatment. Engaging with support groups or counseling can provide additional resources and coping strategies, making it easier to navigate the challenges associated with sleep apnea.